Pheochromocytoma/Paraganglioma
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Unit 1
Dr. Sravya Kandala
Dr. Navya
Dr. Raheem
Dr. Gnanadha
Dr. Chetana
Dr. Ashfaq
Dr. Charan PGY1
Dr. Chandana PGY1
Dr. Sushmitha PGY2
Dr. Aditya PGY3
Dr. Praneeth PGY3
Dr. Praveen Naik Ass. Prof.
Dr. RAKESH BISWAS HOD
Here is a case I've seen:
Admission under Unit 1 on 22/02/2021
40 y/o male came in with c/o neck pain, headache, excessive sweating & palpitations since this afternoon. Went to the local hospital and was diagnosed with hypertensive urgency and was referred to our hospital.
No h/o vomitings, LOC, giddiness and involuntary movements.
No h/o SOB, palpitations, pedal edema
He was diagnosed to have Type II DM a month ago and is currently on Metformin 500mg OD.
No other significant past history.
General Examination
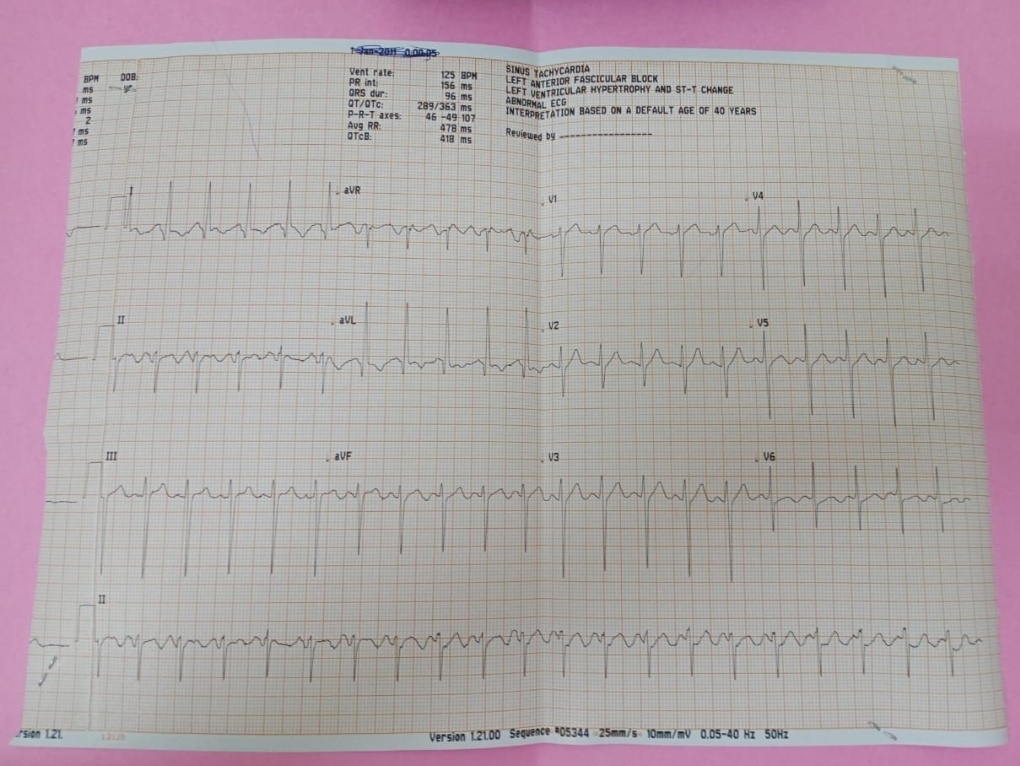
PR - 110bpm
BP - 180/100 mm Hg
Temp - Afebrile
RR - 22 cpm
SpO2 - 99%
CVS - S1, S2 +
RS - Centrally positioned trachea, BAE+ , NVBS
PA - Soft, non-tender, no organomegaly
CNS - NFND
Diagnosis
Denovo HTN secondary to ?Pheo
Treatment
Tab. Nicardia 10mg stat
PR, BP monitoring hourly
BP dropped by itself without any pharmacological intervention.
Discussion:
Causes of secondary hypertension could be Renal or Endocrinal.
Ruling out renal causes
His baseline renal function was intact and he had no bruit in the abdomen, so a clinically significant renal artery stenosis is unlikely.
Ruling out other endocrinal causes
✓The skin thickness on the proximal phalanx of the non dominant hand less than 2mm has a likelihood ratio of 115.6 for detecting Cushings disease and syndrome. That, he didn't have. So cushings is unlikely. (Pituitary)
✓He did not have features of hypercalcaemia - stones (he did have a history of stones for which he was operated), bones, groans and psychiatric overtones and polyuria and constipation. So PTH unlikely.
✓He does not have adrenal excess features like hypokalemia, met alkalosis, gynaecomastia.
✓The key here is the diabetes, the wide fluctuant symptomatic BP and the unusual catecholamine features like sweating, visual disturbances, severe headache, anxiousness and dyspnea.
https://pubmed.ncbi.nlm.nih.gov/7456190/
https://www.nichd.nih.gov/health/topics/factsheets/pheochrom
With a high clinical suspicion of Pheochromocytoma/Paraganglioma, 24 hour Unrinary Fractionated Metanephrines were sent.
Result
Interpretation of the Results
https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/83006
METANEPHRINE
Males
Normotensives
3-8 years: 29-92 mcg/24 hours
9-12 years: 59-188 mcg/24 hours
13-17 years: 69-221 mcg/24 hours
> or =18 years: 44-261 mcg/24 hours
Reference values have not been established for patients that are <36 months of age.
Hypertensives: <400 mcg/24 hours
NORMETANEPHRINE
Males
Normotensives
3-8 years: 34-169 mcg/24 hours
9-12 years: 84-422 mcg/24 hours
13-17 years: 91-456 mcg/24 hours
18-29 years: 103-390 mcg/24 hours
30-39 years: 111-419 mcg/24 hours
40-49 years: 119-451 mcg/24 hours
50-59 years: 128-484 mcg/24 hours
60-69 years: 138-521 mcg/24 hours
> or =70 years: 148-560 mcg/24 hours
Reference values have not been established for patients that are <36 months of age.
Hypertensives: <900 mcg/24 hours
✓Pt. is fitting into every aspect here, 2x upper normal limit for his age & also more than 900 mcg/24 hrs.
TOTAL METANEPHRINE
Males
Normotensives
3-8 years: 47-223 mcg/24 hours
9-12 years: 201-528 mcg/24 hours
13-17 years: 120-603 mcg/24 hours
18-29 years: 190-583 mcg/24 hours
30-39 years: 200-614 mcg/24 hours
40-49 years: 211-646 mcg/24 hours
50-59 years: 222-680 mcg/24 hours
60-69 years: 233-716 mcg/24 hours
> or =70 years: 246-753 mcg/24 hours
Reference values have not been established for patients that are <36 months of age.
Hypertensives: <1,300 mcg/24 hours.
✓The upper limit of normal for his age for total 24h urine metanephrines (metanephrines + normetanephrines) is 646 and he has almost 3x those levels doesn't he. In any case, even if we consider him as a hypertensive, he has total levels above 1300.
✓Total Metanephrine levels in our patient is around 1945.98 much/24 hrs , so he requires further radiological investigations.
Current diagnostic imaging of pheochromocytomas and implications for therapeutic strategy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5840941/
Readmission on 03/03/21
40 y/o male came to the OP with complaints of paroxysmal headaches since 2 years, Abdominal pain since 2 years, Profuse sweating since 2 years, Palpitations since 2 years.
Patient was apparently asymptomatic 2 years ago and then developed Paroxysmal headache associated with profuse sweating & abdominal pain not a/w nausea & vomitings.
He is an occasional alcoholic and non smoker, irregular bowel movements.
K/C/O Diabetes since 2 months.
No significant family history.
General Examination
No signs of Pallor, Icterus, Cyanosis, Clubbing, Generalized lymphademopathy, Pedal edema.
Vitals
PR - 80 bpm
RR - 16 cpm
BP - 160/80 mm Hg
Temp - Afebrile
Grbs - 120mg/dl
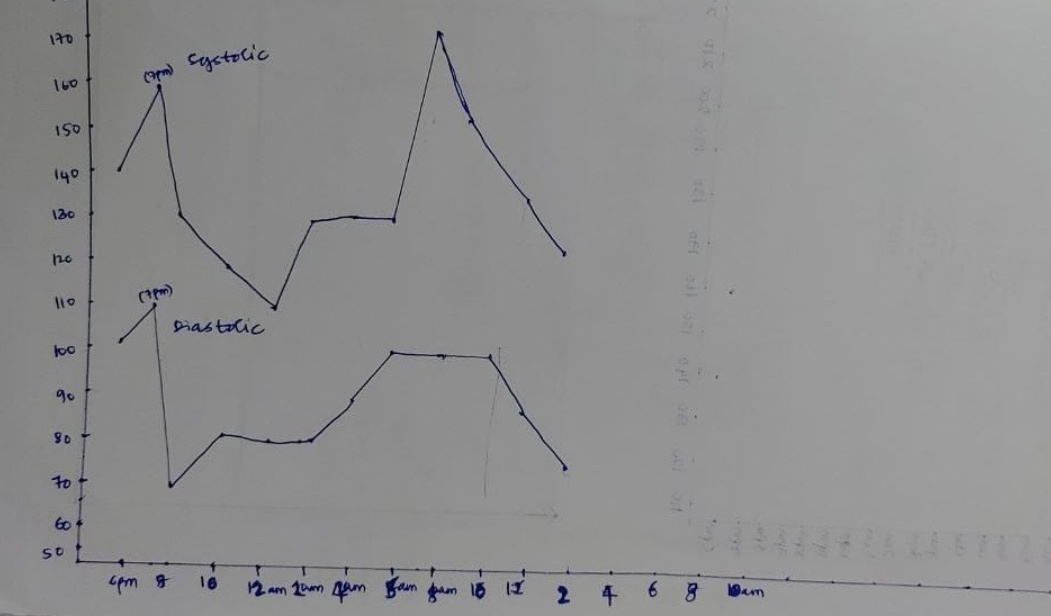
(22/2/21 - 23/2/21 & 3/3/21 - 6/2/21)
CVS - S1, S2 +
RS - Centrally positioned trachea, BAE+ , NVBS
PA - Soft, non-tender, no organomegaly
CNS - NFND
Treatment
1. Salt restricted diet
2. Fluid restriction
3. GRBS monitoring 4th hourly
4. BP/PR monitoring 4th hourly
Adviced CT Renal Angio.
Previous admissions
One admission (21st January 2021) - under Unit 4
Patient had complaints of chest pain (pricking type radiating to his left arm) at 4 am in the morning a/w h/o alcohol intake and consumption of spicy food the previous night .
h/o similar complaints in the past - 2 episodes of chest pain, palpitations and uneasiness (1 episode in 2019 & the other in 2020).
h/o fever with chills since 10-15 days (widal positive) - relieved with medication
No h/o vomitings, loose stools, SOB, palpitations.
Investigations
Urine sugars ++++
USG - Grade 1 Fatty Liver
✓Key here is chest pain, palpitations & uneasiness in 2019 & 2020. No hypercalcemia either.
✓FBS > PLBS suggests something attacking him more in the early hours of the day.