45 y/o male with abdominal pain and vomitings since 1 week
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Dr. Navya
Dr. Raheem
Dr. Gnanadha
Dr. Chetana
Dr. Ashfaq
Dr. Charan PGY1
Dr. Vamsi PGY1
Dr. Sushmitha PGY2
Dr. Adithya PGY3
Dr. Praneeth PGY3
Dr. Praveen Naik Ass. Prof.
Dr. RAKESH BISWAS HOD
Here is a case I've seen:
Admission under Unit 1 on 15/02/2021
45 year old male presented with complaints of pain abdomen since 1 week, vomitings since 1 week.
Pt was apparently asymptomatic 6 years back then he suddenly developed involuntary movements which were initially focal and later generalised associated with transient loss of consciousness, frothing and tongue bite.
On further interveiw he claims his seizure episode is due to abstinence of alcohol and since then whenever he senses preictal symptoms, he drinks 90ml of whiskey which he carries in his pocket.
He has had 16-17 episodes since then and each episode lasted for 5-10 minutes with post-ictal confusion for about one hour, last episode was 2 months back after his uncles' demise.
H/o abdominal pain since one week which is in the right upper quadrant, burning type of pain, non-radiating associated with vomitings, 2-3 episodes/day, bilious, non projectile, not associated with blood.
Not a K/C/O DM, HTN, TB, CAD, Asthma
Mixed diet.
Disturbed sleep.
Loss of appetite since 1 week.
Known alcoholic since 17 years 90ml whiskey (OC) per day.
Tobacco chewer since 22 years.
Regular bowel and bladder movements
No known allergies.
No significant family history.
General Examination
Patient is conscious, coherent & cooperative.
Vitals
BP 110/70 mm Hg
PR 82 bpm
RR 19 cpm
SpO2 98% at RA
Afebrile
Icterus +
Palpebral conjunctiva appears red.
No signs of Pallor, Cyanosis, Clubbing, Generalized lymphadenopathy, Pedal edema
CVS
No visible pulsations
Left hemothoracic bulge present
S1,S2 heard,loud P2
RV type of apex (diffuse)
Parasternal heave +
RS
BAE+
AP 25cm, TV 20cm
Chest expansion appears to be Rt>Lt, but all areas are expanding equally.
Percussion -
P/A
Soft.
Tenderness in the right hypochondrium, epigastrium and umbilical region.
No engorged veins & no organomegaly
Tympanic note on percussion.
Bowel sounds +
Abdominal circumference - 74cm
CNS
Tone
Normal in both upper limbs.
Hypotonia in both lower limbs.
Power - 4/5 in all limbs
Reflexes. Right. Left
Biceps. 3+. 3+
Triceps 2+. 3+.
Knee. absent. absent.
Ankle. 2+. 2+.
Plantar. Flexor. Flexor
Romberg test - Positive
Vibration
Both LL - 8 sec at ankle
Both UL - 8-10sec at wrist
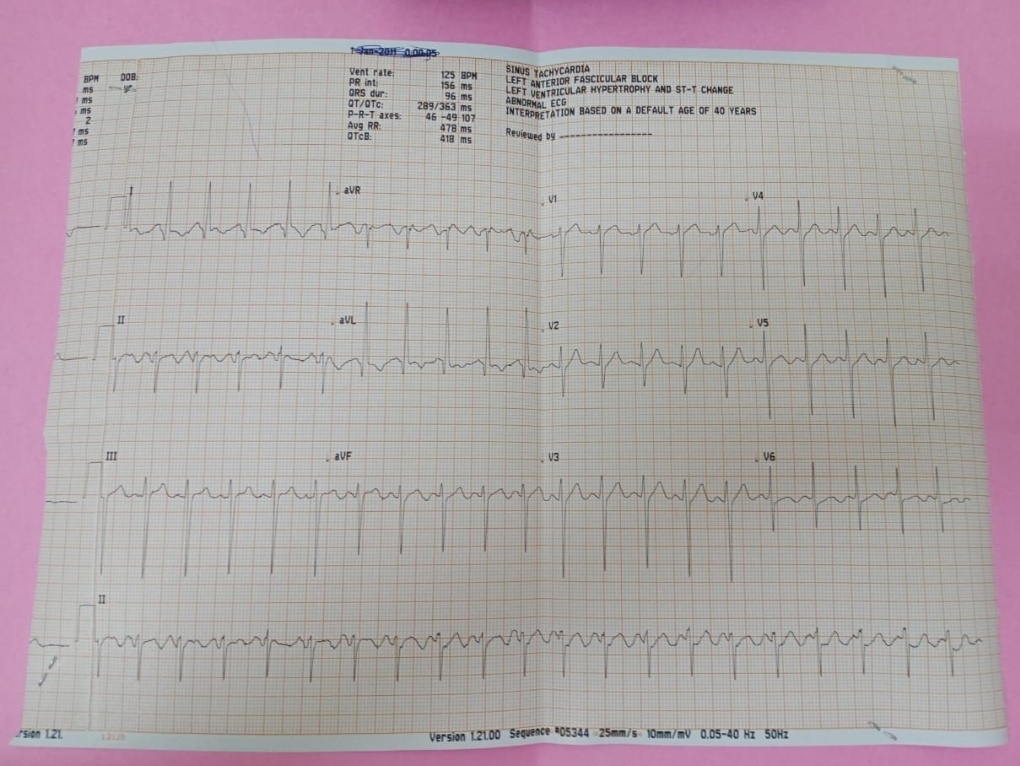
Investigations
Diagnosis
?Acute Alcoholic Hepatitis with thrombocytopenia
?Polycythemia Vera
Treatment
Day 1
IV Fluids - 1 NS, 1 RL
Inj. Optineuron 1 amp in 100 ml NS IV BD
Inj. Zofer 4 mg IV
Inj. Pan 40 mg IV
Tab. PCM 650 mg sos
BP/PR/SpO2 monitoring
Day 2
IV Fluids - 1 NS, 1 RL
Inj. Optineuron 1 amp in 100 ml NS IV BD
Inj. Zofer 4 mg IV
Inj. Pan 40 mg IV
Inj. Thiamine 1 amp in 100 ml NS IV BD
Tab. PCM 650 mg sos
BP/PR/SpO2 monitoring
Day 3
IV Fluids - 1 NS, 1 RL
Inj. Optineuron 1 amp in 100 ml NS IV BD
Inj. Zofer 4 mg IV
Inj. Pan 40 mg IV
Inj. Thiamine 1 amp in 100 ml NS IV BD
Tab. PCM 650 mg sos
Tab. Oxazepam 15 mg OD
Tab. Baclofen-XL 20 mg OD
Tab. Nicotex Gums 2mg sos
BP/PR/SpO2 monitoring
Day 4