Resting Tremor
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Unit 1
Dr. Sravya Kandala
Dr. Navya
Dr. Raheem
Dr. Gnanadha
Dr. Chetana
Dr. Ashfaq
Dr. Charan PGY1
Dr. Chandana PGY1
Dr. Sushmitha PGY2
Dr. Aditya PGY3
Dr. Praneeth PGY3
Dr. Praveen Naik Ass. Prof.
Dr. RAKESH BISWAS HOD
Here is a case I've seen:
Admission under Unit 1 on 03/03/2021.
Introduction :
Parkinson's disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson's.
People with Parkinson's also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many automatic functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson's, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position. Many brain cells of people with Parkinson's contain Lewy bodies, unusual clumps of the protein alpha-synuclein.
Although some cases of Parkinson's appear to be hereditary, and a few can be traced to specific genetic mutations, in most cases the disease occurs randomly and does not seem to run in families. Many researchers now believe that Parkinson's disease results from a combination of genetic factors and environmental factors such as exposure to toxins.
Case discussion :
The patient reports that he first noticed them happening nearly 6 months ago, which was very small in amplitude, affecting these two fingers only. He attests that these movements often worsened with rest and abated with activity. They were not troublesome initially but since the past 2 months he has been unable to correct answer sheets because of the involvement of his thumb and maintaining stability of his hand was proving difficult. He describes these movements as involuntary, rhythmic to and fro oscillations.
He also adds that his handwriting has become ugly with very small letters. On interviewing further, the patient reports that he feels stiffness in his wrists (Right>Left), which has now ascended to his elbows. He says the stiffness is present throughout the range of motion. He also says that since the last 1 month, the same involuntary movements also started appearing in his left hand.
At this point, he also says that his walking has become difficult with small, short steps and a forward stoop, and he feels that although he weighs 60 kgs, he feels like it weighs 100 kgs.
He does not report any difficulty in reading the newspaper, holding the paper, turning pages or folding it back. He does not have any difficulty in brushing his teeth or combing his hair. He also denies having difficulty in holding objects, such as holding a water bottle to drink nor any difficulty in mixing food and eating it. He does not have any difficulty in wearing a vest or in buttoning or unbuttoning of his shirt. No difficulty in lifting his lower limbs and wearing a trouser.
The interview continues and we question for any difficulty in taking the stairs - he reports that he has been having difficulty in taking stairs up, in that he feels he sometimes might lose balance. He has no difficulty in descending stairs. The patient also denies having swaying of his trunk while walking or overshooting his hand while picking up objects.
On pressing further - he reports that he hasn't been having morning erections since 2 months and also reports a loss of sexual desire. He also says that since 2 months his bowel habits have been incredibly erratic, in that he sometimes has an immediate urge to defecate when he has tea and sometimes goes 2 to 3 days with constipation.
He, however, denies feeling dizzy or lightheaded when waking up in the morning. He denies having stiffness in his lower limbs, denies cotton wool sensation of floor, denies burning pain or inability to feel hot or cold stimuli. He also denies buckling of knees but, however, he reports that he has been having a great difficulty to walk in the dark since 2 months and says that he feels like he would definitely fall without support.
His brother gives a positive affirmation for all his symptoms and also says that he previously used to be a fairly jovial and hardworking man with good oratory skills, however, since the last 2 months he says his brother's speech lacks that 'edge' which he previously had. On asking further, the brother says that he has been speaking in a monotonous drab since 2 months.
The patient denies ever having urinary incontinence, memory deficits, the brother vehemently denies the patient ever being anti-social, he does not have any difficulty in forming new memories or any visual deficits.
He has no relevant past or family medical history.
Vitals at the time of history taking -
PR - 88 bpm
BP - 190/110 mm Hg
After standing for 3 mins - BP - 160/110 mm Hg
Temp - Afebrile
RR - 16 cpm
General examination
Patient is conscious, coherent & cooperative.
Vitals
BP - 160/100 mm Hg
PR - 70 bpm
Temp - Afebrile
RR - 20 cpm
No signs of Pallor, Icterus, Cyanosis, Clubbing, Generalized lymphademopathy, Edema.
CVS
S1, S2 +.
Apex beat in 5th ICS on the MCL.
Raised JVP.
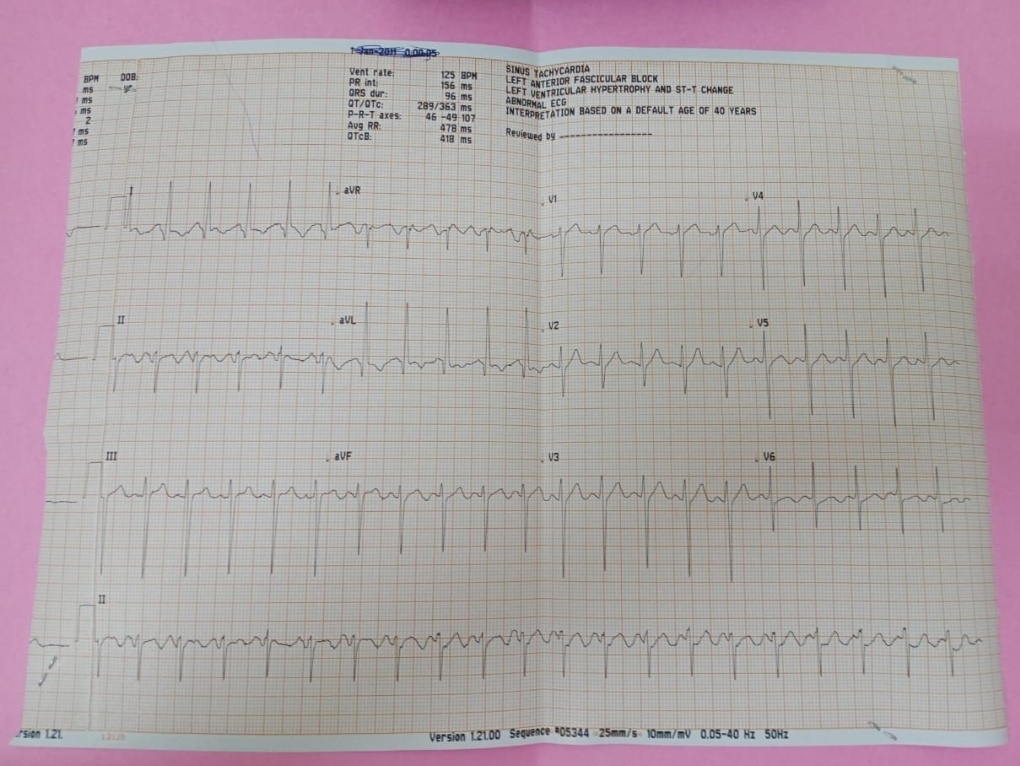
✓Shows Sinus Tachycardia with pseudo infarct pattern in leads I and aVL with dagger q waves in the same leads.
✓No late intrinsicoid deflection of R wave with modified cornell criteria showing LVH.
RS
Shape & symmetry of chest - Normal
Respiratory movements - Equal on both sides
BAE+
NVBS
P/A
Soft, Non-tender
no organomegaly
Bowel sounds+
CNS
HMF
Patient is conscious.
Orientation to time, Place & Person +
Speech and language- normal
Memory - intact
MMSE
29/30 (No cognitive impairment)
CN Examination
1st
Normal (smell of soap).
2nd
Counting fingers at 6mts both eyes normal.
3rd,4th,6th
Pupil size. N N
DLR/CLR. N. N
No pstosis, nystagmus.
5th
Both sensory & motor normal.
Corneal & Conjunctival reflex +.
7th
Nasolabial fold normal.
No deviation of mouth.
Salivation & Lacrimation unaffected.
8th
Rinne's AC>BC.
Weber's - No lateralization.
9 th, 10th &
Palatal movements normal.
No difficulty in swallowing.
Gag reflex present.
11th
Movements of neck in all directions+.
Lifting of shoulders +.
12th
Tone of tongue - Normal.
No wasting, no fibrillations & deviation of tongue.
Tongue tremor+.
MOTOR SYSTEM
Right. Left
✓Bulk Normal Normal
✓Tone
Upper limb R. L
Shoulder Normal Normal
Elbow Normal Normal
Wrist Hypertonia Normal
(Cog wheel rigidity)
Lower limb Normal Normal
✓Power
UL
Proximal 5/5 5/5
Distal 5/5 5/5
LL
Proximal 4/5 4/5
Distal 5/5 5/5
✓Reflexes
Superficial reflexes
Right Left
Corneal + +
Conjunctival + -
Abdominal + -
Plantar - -
Deep tendon reflexes
Right Left
Biceps 2+ 2+
Triceps 2+ 1+
Supinator 1+ Absent
Knee 3+ 3+
Ankle 1+ 1+
Clonus Absent. Absent
Involuntary movements - Resting tremors of Right upper limb , 3-4Hz, low amplitude.
Gait - Reduced arm swing.
Finger tap and toe tap - Normal.
No decrease in speed on repeating the movement continuously.
✓SENSORY SYSTEM
Right Left
Pain + +
Fine touch + +
Temperature + +
Vibration
Medial malleolus 5.7s 4.6s
Patella 9s 4.3s
Elbow 4.8s 6.4s
Wrist 5s 7s
Propriception Normal Normal
Stereognosis Normal Normal
✓CEREBELLUM
Titubation - absent
HINTS
Head Impulse - negative
Nystagmus - negative
Test for skew - negative
Gait Ataxia absent.
Dysarthria absent.
Rebound phenomenon absent.
Intentional tremors - absent.
Pendular knee jerk - absent.
Tandem walking normal.
Coordination tests
Dysdiadochokinesia absent
Finger nose test normal
Heel knee test normal
Rombergs Test - Negative
Micrographia +
✓Findings - The movements in the right lower limb is slower than the movements in the left lower limb.
✓The first test was only toe tapping, the second test is entire foot tapping.
Rapid supination and pronation - Diadochokinesia
✓MENINGEAL SIGNS
Neck stiffness - Absent
Kernig's sign - Negative
Brudzinski's sign - Negative
✓AUTONOMIC
Postural hypotension+(Supine - 180/110, Standing 160/90).
Resting tachycardia absent(PR 80/min,regular)
Abnormal sweating absent.
H/O erectile dysfunction+.
Problem Representation -
A middle aged man presenting with a 6 months history of gradually progressive, asymmetric rest tremor with autonomic features is provisionally diagnosed with
1. Idiopathic Parkinson's Disease Stage 1 with denovo HTN.
2. Multiple System Atrophy - Parkinsonian Type (MSA-P).
Treatment
1. Tab. Syndopa Plus 125 mg QID
2. Tab. Syndopa 125 mg CR OD
3. Tab. Telma 40 mg OD
4. 4th hourly BP/PR/Temp monitoring
Prognosis of Stage 1
Stage 1 is the mildest form of Parkinson’s. At this stage, there may be symptoms, but they’re not severe enough to interfere with daily tasks and overall lifestyle. In fact, the symptoms are so minimal at this stage that they’re often missed. But family and friends may notice changes in your posture, walk, or facial expressions.
A distinct symptom of stage 1 Parkinson’s is that tremors and other difficulties in movement are generally exclusive to one side of the body. Prescribed medications can work effectively to minimize and reduce symptoms at this stage.